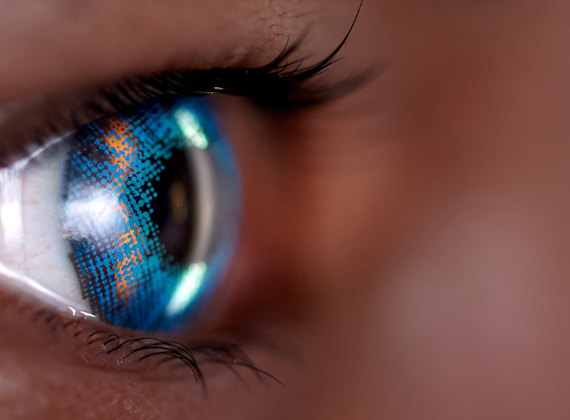
School of Optometry and Vision Sciences
We train the next generation of optometrists, and our innovative research has advanced global understanding of vision disorders to improve quality of life worldwide. We work alongside local and global communities to deliver the best eye care and pioneer advancements in eye health.
Our new MOptom programmes provide you with the scientific and clinical knowledge to register as an optometrist with the General Optical Council.