Scientists shed new light on how SARS-CoV-2 evades the immune response in early infection
19 July 2022
A new study led by Cardiff University has shed light on how the COVID-19 virus “interferes” with the body’s initial immune response to avoid detection.
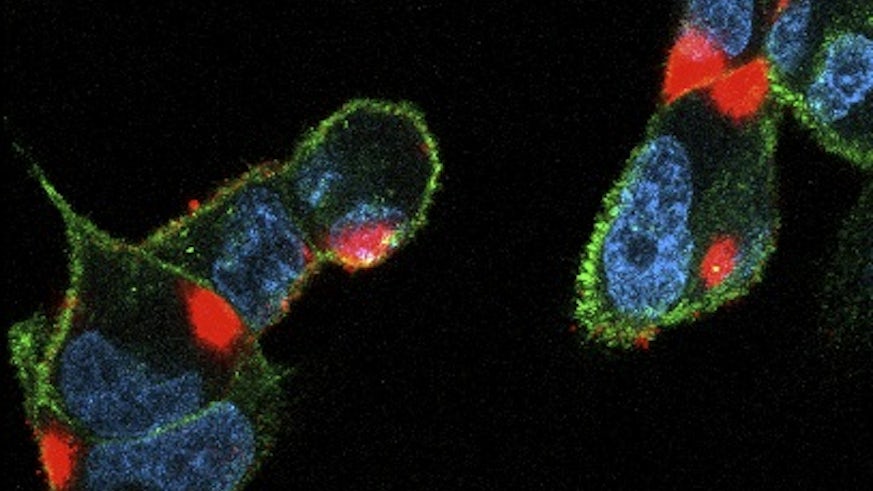
In the lab scientists showed how SARS-CoV-2 can evade natural killer (NK) cells – a type of white blood cell and a crucial part of the early immune response – by shutting off several ways these cells recognise the virus.
However, they also found the virus is unable to dodge NK cells that have been activated by antibodies to recognise viral proteins on the infected cell – meaning their findings, published in the journal eLife, could have important implications for vaccine design.
“Our research suggests vaccines could be improved and bolstered to ensure we better equip the body’s own defences to attack the virus,” said lead author Dr Ceri Fielding, a Lecturer from Cardiff University’s School of Medicine.
The innate – or initial – immune response to COVID-19 is a crucial but complex process and the virus has a broad range of strategies to avoid being detected. In the initial immune response, NK cells recognise viral targets through stress-induced molecules on the surface of infected cells.
As part of the adaptive – or more powerful, longer lasting – immune response, they then recognise infected cells by harnessing virus-specific antibodies. This mechanism is known as antibody-dependent cellular cytotoxicity (ADCC).
The team screened proteins expressed on the surface of infected cells to show how the virus evades NK cells by preventing the synthesis of several molecules, known as ligands, that bind to its receptors. Further experiments revealed viral proteins Nsp1 and Nsp14 could be responsible for that effect.
They then showed how NK cells could be triggered by antibodies bound to SARS-CoV-2 infected cells, via the ADCC mechanism, marking out the cell for destruction.
In most of the current vaccines, the spike protein is used as the key component – but this study suggests other viral proteins would induce different aspects of the immune response.
“We found that although natural infection induces these antibodies well, vaccination does not – this is because the targets for the antibodies are not in the vaccines we use currently,” said Professor Richard Stanton, a virologist also from Cardiff University’s School of Medicine.
“As we look towards next-generation coronavirus vaccines, our work provides a way to enhance their efficacy, by inducing the right type of antibodies that can attack and kill the virus.
“Specifically, viral proteins which induce antibodies capable of ADCC in natural killer cells could be added to current formulations. Further studies are now needed in vivo to more fully explore this.”
Dr Fielding added: “Current vaccines work well and should be taken up by people, but our research indicates a way to enhance the next generation of therapeutics.”
This work was funded by the Welsh Government's Ser Cymru Tackling COVID-19 scheme and the UK Coronavirus Immunology Consortium.

