Project Sepsis
A research project aiming to harness the immune system and its soft wiring to metabolism as a detector of infection.
Project Sepsis is a research collaboration across medicine and science disciplines that addresses an urgent medical need for recognising and accurately detecting infection underlying sepsis - “blood poisoning” - in extremely vulnerable populations of the very young and old.
Symptoms can be subtle, yet if sepsis goes undetected, catastrophic loss of life can occur within hours if not prescribed antibiotics. Consequently there is an overuse of antibiotics that can lead to antimicrobial resistance, itself a global health threat. The sensitivity of current tests is poor with between 6 to 8 cases out of 10 being missed.
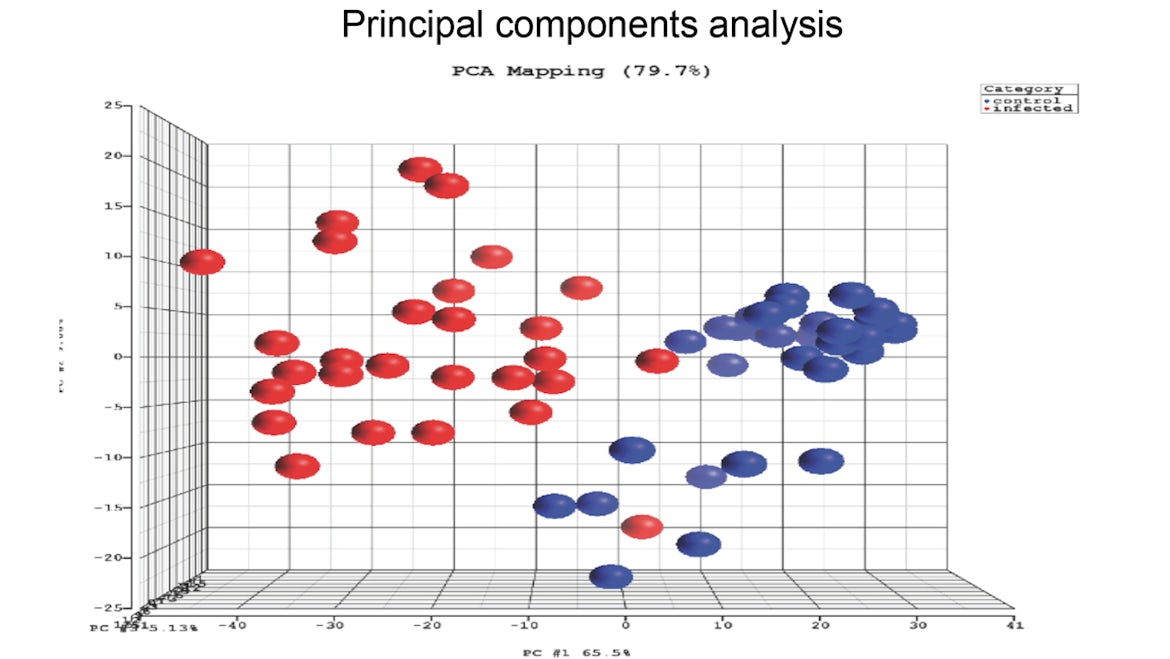
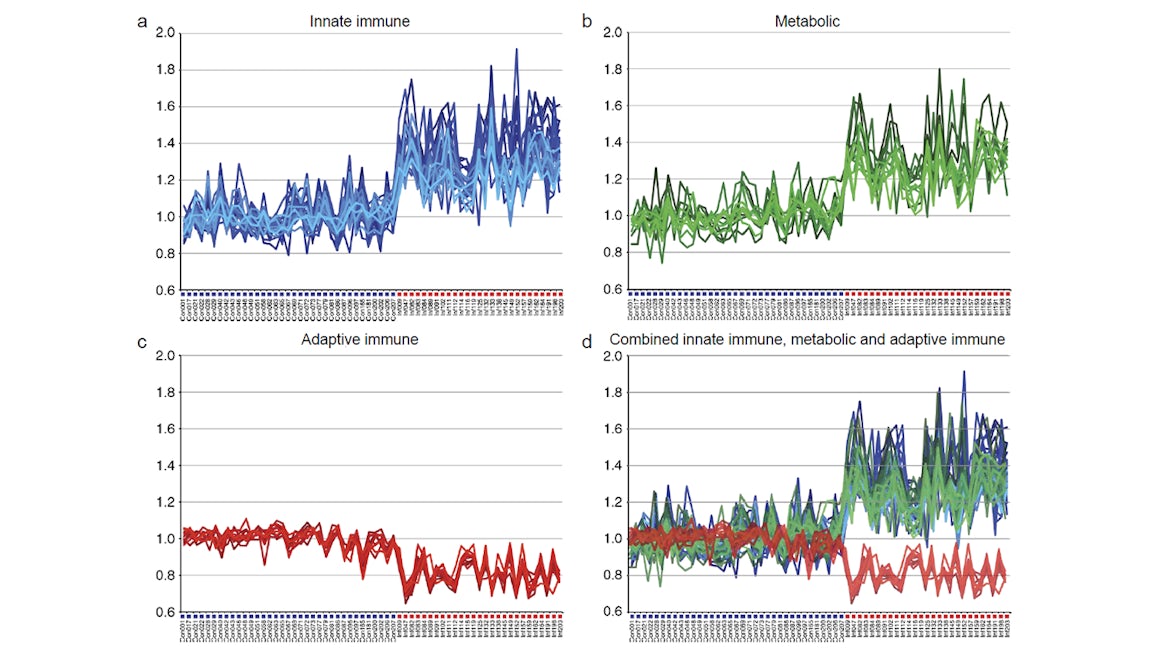
Project Sepsis uses computer-assisted genome, proteome, and metabolism approaches to decode the communication from the blood-immune system to more rapidly detect infection and identify innovative treatments.
Project Sepsis is part-funded by the European regional Development Fund through the Welsh Government.
If you would like to find out more about project sepsis please contact: projectsepsis@cardiff.ac.uk
Project Sepsis is part of a collaboration with Dr C Costello’s team at Imperial College which recently secured National Institute for Health Research (NIHR) funding for a project tilted: Digital alerting to improve sepsis detection and patient outcomes in NHS Trusts.
Through this collaboration, the Project Sepsis team facilitated that our research partner, Cardiff and Vale University local health board, become a member of the NIHR Health Informatics Collaborative (HIC) data sharing framework.
This will support the establishment of a sustainable clinical informatics infrastructure at the trust in line with those at other participating HIC centres, create a shared governance framework and enable collaborative clinical research projects across the HIC, with all centres involved in relevant collaborations and initiating expansion to future data collaborations.
Celebration of achievement
Project Sepsis was funded by the Welsh Government’s Sêr Cymru programme. Prof Peter Ghazal was appointed Sêr Cymru Chair in Systems Medicine, Systems Immunity Research Institute, and established Project Sepsis in December 2017 to strengthen sepsis and systems research within Cardiff University and Wales. The project has produced high quality and impactful research, with substantive progress being made in the fight against Sepsis and improving sepsis awareness with the Sepsis Trust UK, and management and diagnosis, while increasing research capacity and our understanding of what drives this condition.
Project Sepsis applied a community-in-action approach uniquely establishing a Sepsis Engagement Centre housing the “Goldilocks Ward” used for promoting public and patient involvement, training and research. We successfully appointed at an early stage a lay advisory group, and over 20 research staff and 8 research students including 2 new lectureships that actively contributed to the project, and have strengthened collaborations with existing partners while building national and international research networks and links with new strategic partners from multi-disciplinary teams across academy and industry. This includes: Introduction of a sepsis case study to the medical curriculum, working with industry to develop a 360 degree fully immersive virtual reality training resource for medical students and staff, mathematical models for understanding and predicting sepsis, validating and developing new diagnostic tools and tests. Across three of our clinical platforms (neonatal, maternal and paediatric sepsis studies) we gratefully received blood samples from approximately 1000 participants in our research at Cardiff and Vale University Hospital and almost similar contribution from our partnering centres. This was during very challenging circumstances during the pandemic, allowing us to establish a large biobank of samples for continued research, while building key relationships with our clinical teams across various specialities in the NHS.
We are now beginning to see an increase in scientific out puts and collaborations with other UK based and international institutions. Our research and technical achievements of Project Sepsis, could not be accomplished without participation of public and patient involvement. Improved public awareness of sepsis is key and we are proud of our contributions to a variety of successful engagement events highlighting differing aspects of sepsis and including yearly seminars to mark World Sepsis Day. As a whole community we have increased the development of excellence research capability in Wales within systems medicine, and although the European sponsored Ser Cymru programme ends in April 2023, Project Sepsis will continue with the next phase of decoding sepsis and continue to build on our achievements.
Prof Peter Ghazal was recognised in the New Year’s Honours 2023 and awarded an OBE for his services to systems immunology.
Research
Key research themes
(see Figure 1)
- Maternal sepsis (mSEP)
- Neonatal sepsis (nSEP)
- Paediatric sepsis (pSEP)
- Adult sepsis (aSEP)
Areas of expertise
Core Project Sepsis team
Prof Peter Ghazal (n,p,aSEP) - Chief Investigator and academic lead for n, pSEP
My research interests are aimed towards understanding how host-gene networks control infection, especially with those host-pathways associated with sepsis and the immune-metabolic axis. My recent studies have pioneered the field of host genomics of early-life infection, mapping and deciphering gene metabolic signatures of systemic host response to infection in pre-term infants and neonates and understanding the molecular wiring and mechanisms for coupling lipid metabolism to immune (interferon) response.
These studies are specifically aimed at the development of new diagnostic and therapeutic strategies, including predictive modelling of host-defence against infection in sepsis, and the development of new computational and functional genomic methods for gaining a deeper understanding of complex dynamical biological systems of viral (cytomegaloviral) and microbial diseases.
Prof Valerie O’Donnell (n,p,aSEP) - Principle Investigator and academic lipid metabolism lead
Our current research is focused on understanding the role of lipids (fats) in vascular inflammation, a major complicating factor in sepsis and driver of multi-organ failure. Lipids are generated by circulating blood cells and platelets in response to blood infection. These stimulate clotting and cell damage, and dampening these processes while allowing the body to control the infection itself is a major goal of our research.
We have identified large numbers of new lipids made in blood cells and understanding their biological functions is a core research goal. Delineating how lipids and energy metabolites interface during sepsis to control inflammation and blood clotting is essential if we are to develop new prevention and treatment approaches.
Dr Robert Andrews (n,p,aSEP) - Informatics lead
My interests are in the information management and analysis of large biomedical datasets. As part of my role, I design and build compute infrastructure for handling high-throughput ‘big-data’. Specifically, project sepsis will deploy a biomedical informatics framework for the capturing, querying, retrieval and sample tracking of clinical and laboratory research information with which to automate and manage novel microfluidic approaches aimed toward advancing innovative precision diagnostic tests and treatments for sepsis.
I also teach chromatin informatics with the Wellcome Trust advanced courses and lead the omics module on the MSc in Bioinformatics at the University.
Sarah Edkins
Dr Daniel White - Senior Innovation and Technology Scientist
With over 20 years of experience in lipid biology and analytical chemistry, spanning scientific fields from environmental monitoring to biomedical research, my role role in Project Sepsis is to develop high-throughput lipidomic profiling strategies to determine robust biomarkers of sepsis in the systemic circulation of patients. These methods are part of integrative strategy for understanding the casual link between metabolism and the immune response in determining sepsis patient outcome and together with clinical team members will be translated to the clinical care pathway for improving precision in identifying and treating those patients presenting with suspected sepsis.
Dr James McLaren - Sêr Cymru Lecturer in Systems Immunity
My research interests focus on understanding how adaptive immune responses (T cell driven) are mobilised during viral (HIV, cytomegalovirus) and microbial infections, inflammation and disease. Furthermore, I have a keen interest in discovering how this type of cellular immunity is regulated by biological signals (cytokines) and how it can destabilise when global immune responses become imbalanced, such as in sepsis. As part of Project Sepsis, my aim is to deconvolute the immunological mechanisms that drive the suppression of adaptive immunity in sepsis with a view to help improve diagnosis and to inform the design of novel therapeutic interventions.
Dr. Nicos Angelopoulos - Sêr Cymru Lecturer in Computational Systems Immunity
I work on knowledge based systems for explainable AI in biology and medicine. A computer scientist by training, I worked on methodological aspects of probabilistic programming before developing a strong interest in knowledge-based data analytics in bio-medicine. Of particular interest is the representation of biological knowledge in the context of machine learning both in how prior knowledge can incorporated in the learning process, but also in how we can learn models of interpretable knowledge. Bayesian approaches to model learning are of particular interest, especially when combined with classical AI approaches of knowledge representation amalgamating logic and probability theory. I also have interests in open source software and the ethical use of AI, contributing a number of libraries to the SWI-Prolog, logic programming system.
Dr Luke Davies
I am a passionate scientist with a research background in innate immune cell biology and metabolism. Sepsis is a life-threatening condition driven by dysregulated immunity which results in organ failure and metabolic dysfunction. I am excited to work with Project Sepsis to investigate new diagnoses and treatments for sepsis.
Dr. Patricia Dos Santos Rodrigues
Dr Jason Twohig - Lecturer in Medical Transcriptomics
I utilise novel ‘OMICs’ approaches to facilitate the identification and stratification of patients with chronic disease for effective therapeutic treatment with biologics. I am particularly interested in identifying blood transcriptomic signatures which predict the presence of SEPSIS, its progress, its mechanism, and its resolution. More broadly, my research interests also include understanding the role of cytokines in inflammation and homeostasis in the immune and neurological system during development and infection.
Dr Widad Dantoft (n,p,aSEP) - Research Associate
My research interest lies in understanding the intricate interplay between immunity and metabolism in the presence of viral (CMV) and bacterial infections, and how this affects the infection process and outcome. I am in particularly interested in how this immune-metabolic interplay is regulated on a transcriptional level.
Dr Mallinath Chakraborty (nSEP) - Clinical lead
My interests are in neonatal respiratory medicine and sepsis. I am the local Principal Investigator for several multi-centre clinical trials and am developing my own research group. I also run the respiratory module of the Masters in Neonatal Medicine at Cardiff University.
Dr Summia Zaher (mSEP) - Clinical lead
Dr Tamas Szakmany (aSEP) - Clinical lead
In collaboration with Public Health England and industry (Randox and Atlas Genetics) I have led Innovate UK funded multicentre clinical trials on adult sepsis. These studies identified mRNA and protein biomarker panels that distinguish sepsis from non-infective origin of organ dysfunction for use with point-of-care devices.
I further designed and led an award winning (Cardiff University Excellence in teaching award 2017 and NHS Wales Award runner-up 2016) collaboration with the Cardiff University Research Society for medical students, establishing the burden of sepsis on the general wards and Emergency Departments in Wales. These multi-centre point-prevalence studies recruited over 1000 patients quantifying the incidence when using different clinical scores to define sepsis.
Dr Siva Oruganti (pSEP) - Clinical lead
Linda Moet
My background is a Bachelor in Medical Biology and a Master in Biomedicine. What fascinates me most is how complex systems in the body are regulated and interact, especially the immune system and the gut microbiota. My PhD is focused on the G-Protein coupled receptor (GPR) 84. This receptor has only been discovered quite recently; it is present on various immune cells and binds medium chain fatty acids. These come (most likely) from breast milk in the neonatal context. The receptor thus connects metabolism and diet with immunity. Since its expression is upregulated during neonatal sepsis, we decided to investigate the role of GPR84-signalling during neonatal sepsis, the presence and effects of its ligands and their potential origins. Hopefully this project will further the understanding of sepsis leading to better diagnosis and treatment in the future.
Simran Sharma
I am very excited to be joining project sepsis as a clinician as I see the detrimental impact of sepsis on mothers and babies every day. An opportunity to learn more through research is something I am very much looking forward to.
Dr Fergus Hamilton
Freya Shephard
Other collaborators and affiliated team members
Dr Claire Smith (nSEP) - Edinburgh
My research interest is in neonatal infection with on-going involvement in studies in this area. I am actively involved in the local neonatal unit infection surveillance programme and have played a significant part in introducing a successful infection reduction programme to the neonatal unit.
Prof Timothy Walsh (n,pSEP) - Principle Investigator
I am director of BARNARDS, a BMFG funded project examining the burden of neonatal sepsis in Nigeria, Pakistan, Bangladesh, Rwanda and Ethiopia. I am also PI of DETER-XDR-China and CUT-SEC that examines the one health approach to studying AMR in China, Vietnam and Thailand.
I am an advisor on AMR to the United Nations, Médecins Sans Frontières and the Fleming Fund.
Prof B Paul Morgan - Principle Investigator
I am an expert in the complement system, a critical component of innate immunity and a powerful driver of inflammation. Dysregulation of the complement system has been implicated in sepsis and systemic inflammatory response syndromes; indeed, complement markers in blood have been used to predict and monitor these conditions. Critically, an emerging wave of anti-complement drugs may provide new ways of breaking the cycle of inflammation in patients with sepsis.
Dr Paul Morgan (aSEP) - Principal Investigator
As an Intensive Care consultant and the Lead Volunteer in Wales for the UK Sepsis Trust, sepsis makes up a substantial part of my work.
My interests in sepsis has led me to try to drive change in sepsis recognition and care outside the critical care environment, working with staff from primary and secondary care so that sepsis can be spotted early, enabling timely intervention and thereby reduce the need for critical care admission. Ultimately, my hope is that this will reduce not just mortality from sepsis but also the morbidity, which results in long-term health problems for sepsis survivors. I am a member of the steering committee and co-author of the papers that have been published from the Size of Sepsis in Wales and the Defining Sepsis in the Wards point prevalence studies.
Dr Matthias Eberl (aSEP) - Principle Investigator and Academic lead of aSEP
My interdisciplinary research aims to characterise early immune responses in acutely ill patients and define pathogen-specific signatures of cellular and soluble biomarkers ('immune fingerprints'). This work has direct implications for improved diagnosis and treatment of microbial infections including sepsis.
Dr Matthew Morgan (aSEP) - Clinical lead
Intensive care doctor, scientist, computer programmer, teacher and geek interested in machine learning, medical education and public engagement. My PhD used artificial intelligence to tease out “immune fingerprints” from different types of life-threatening infections.
I have spent time training in the UK, Australia and the military. Passionate about critical care medicine and intensive care research, I also work with the British Medical Journal to improve medical education, healthcare IT and research outcomes.
Rhian Thomas-Turner (n,p,aSEP) - R&D Operations Manager
I am the R&D Operations Manager for the Noah’s Ark Children’s Hospital for Wales. My role involves both the strategic and operational oversight of research within the Children’s Hospital and running the newly establish Children and Young Adults’ Research Unit. The aim of the Unit is to act a hub for high quality Child Health research in Wales.
Dr Jenna Bowen - Lecturer, Cardiff School of Pharmacy and Pharmaceutical Sciences
My research interests lie in the field of sepsis and infection, with a particular focus on the development of bio-sensing systems to enable rapid diagnosis, patient stratification and personalisation of therapies. I enjoy working across disciplines and have established collaborations across life science and engineering / physical science disciplines as well as with end-users from the clinical, commercial and third sector in order to deliver fit-for-purpose technologies.
I am also a co-founder of a start-up company, Cotton Mouton Diagnostics (CMD), which is developing a diagnostic platform that can be deployed across a range of healthcare settings.
Dr Mario Labeta (aSEP) - Senior Lecturer
My current work focuses on the immunobiology of the Toll-like family of immune receptors (TLRs) as mediators of immune and inflammatory responses. Following our discovery of a soluble form of TLR2 (sTLR2) in blood that has anti-inflammatory capacity, we are evaluating whether plasma sTLR2 may be used as a biomarker for sepsis, as opposed to SIRS and other serious infections. In collaboration with a Welsh biotech company (JRBiomedical, Glyndwr University) we are developing a fast point-of-care test to determine plasma levels of sTLR2.
In further work we have identified TLR2-derived peptides capable of boosting the immune response of immunosuppressed sepsis patients ex vivo, and currently seeking to stratify sepsis patient subgroup(s) that may therapeutically benefit from our TLR-based peptide strategy.
Dr Philip Anyanwu - Lecturer in Public Health
I am an infectious disease epidemiologist with research interests in causal inferential analysis and investigating the mechanism of impact of interventions to address antimicrobial resistance and sepsis.
I have a specific interest in the development and evaluation of digital applications for the management of sepsis, especially in LMICs. I am a co-investigator of a project on maternal sepsis working with research partners from Imperial College London and the University of Ibadan Nigeria to develop a digital system for sepsis alert and monitoring ward movement in maternity patients in Nigeria.
Rebecca Milton - Research Associate - Trial Manager
My research interests lie within maternal and neonatal health and I have a strong interest in working in low- and middle income countries. I obtained my Masters in Public Health at Cardiff University whilst working within a microbiology research group in the Institute of Infection and Immunity, Cardiff University. To date, much of my research has been focused on neonatal sepsis in LMICs. I have been working with Project Sepsis looking immunological markers, risk factors and incidence of stillbirths in northern Nigeria with an additional focus on cultural belief and understanding around stillbirth. I am currently working on a PhD by publication focusing on maternal and neonatal health in LMICs.
A feasibility study of stillbirths in Kano, Northern Nigeria.
Stillbirth Feasibility Study - Video
Our international community
Professor Tobias Strunk (nSEP) - Clinical Associate Professor, Centre for Neonatal Research and Education (The University of Western Australia, Perth, Australia) and Neonatal Directorate, King Edward Memorial Hospital (Perth, Australia)
My research interest is the immunological determinants of newborn susceptibility to invasive bacterial infection and novel prophylactic and therapeutic interventions to reduce disease burden, areas highly relevant to the current proposal.
EU NeoVanc Project
Clinical trial assessing the dosage of vancomycin antibiotic in the treatment of late onset bacterial sepsis caused by vancomycin susceptible bacteria in neonates and infants aged under three months.
Breathing Together
A five year research and engagement programme exploring breathing and lung health in children.
The Theirworld Edinburgh Birth Cohort
A 25-year study to learn more about how being born too soon or too small affects people’s health in later life.
Digital Alerting for Sepsis (DiAlS)
The DiAlS study will investigate the impact of digital sepsis alerts on patient outcomes and staff activity in NHS hospital Trusts across England and Wales.
GCRF
DISCOVER (DIagnostic and Severity markers of COVID-19 to Enable Rapid triage) study
Focused on blood-based biomarkers and their ability to predict a patient’s disease course alongside demographic factors such as age, sex, frailty and other medical conditions.
Project members
- Prof Carlo Giaquinto (University of Padova, Head of Paediatrics AIDS centre, Italy)
- Profs Mike Sharland (St. Georges, University of London, Head of Paediatrics, UK)
- Prof Paul Heath (St. Georges, University of London, Paediatric infectious diseases, UK)
- Prof EvelyneJacqz-Aigrain (Robert Debre Hospital, Head of Paediatric pharmacology, France)
- Prof Irji Lutsar (University of Tartu, Head of Department of clinical microbiology, Estonia)
- Prof. Baiardi (Consorzio per Valutazioni Biologiche e Farmacologiche, Director Biostatistics, Italy)
- Dr. Mark Turner (University of Liverpool, Consultant neonatologist, UK)
- Prof Peter Ghazal (University of Edinburgh & University of Cardiff medical schools, Chief investigator project-sepsis)
Publications
- Milton, R. et al. 2021. Establishing the safety of waterbirth for mothers and babies: a cohort study with nested qualitative component: The protocol for the POOL study.. BMJ Open 11 (1) e040684. (10.1136/bmjopen-2020-040684)
- Milosevic, S. et al. 2020. Factors influencing water immersion during labour: qualitative case studies of six maternity units in the United Kingdom. BMC Pregnancy and Childbirth 20 (1) 719. (10.1186/s12884-020-03416-7)
- Milosevic, S. et al. 2019. Factors influencing the use of birth pools in the United Kingdom: Perspectives of women, midwives and medical staff. Midwifery 79 102554. (10.1016/j.midw.2019.102554)
- Dantoft, W. et al. 2017. Genomic programming of human neonatal dendritic cells in congenital systemic and in vitro cytomegalovirus infection reveal plastic and robust immune pathway biology responses. Frontiers in Immunology 8 1146. (10.3389/fimmu.2017.01146)
- Zhang, J. et al. 2017. Machine-learning algorithms define pathogen-specific local immune fingerprints in peritoneal dialysis patients with bacterial infections. Kidney International 92 (1), pp.179-191. (10.1016/j.kint.2017.01.017)
- Raby, A. et al. 2017. Toll-like receptors 2 and 4 are potential therapeutic targets in peritoneal dialysis-associated fibrosis. Journal of the American Society of Nephrology 28 (2), pp.461-478. (10.1681/ASN.2015080923)
- Holst, B. et al., 2017. Soluble toll-like receptor 2 is a biomarker for sepsis in critically ill patients with multi-organ failure within 12 h of ICU admission. Intensive Care Medicine Experimental 5 (1)(10.1186/s40635-016-0116-z)
- Hopkinson, J. B. et al. 2016. People with dementia: what is known about their experience of cancer treatment and cancer treatment outcomes? A systematic review. Psycho-Oncology 25 (10), pp.1137 -1146. (10.1002/pon.4185)
- Liuzzi, A. R. et al. 2016. Unconventional human T cells accumulate at the site of infection in response to microbial ligands and induce local tissue remodeling. Journal of Immunology 197 (6), pp.2195-2207. (10.4049/jimmunol.1600990)
- Courtier, N. et al. 2016. Cancer and dementia: an exploratory study of the experience of cancer treatment in people with dementia. Psycho-Oncology 25 (9), pp.1079-1084. (10.1002/pon.4212)
- Raby, A. and Labeta, M. 2016. Therapeutic boosting of the immune response: turning to CD14 for help. Current Pharmaceutical Biotechnology 17 (5), pp.414-418. (10.2174/1389201017666160114095708)
- Duffin, R. et al., 2016. Prostaglandin E2 constrains systemic inflammation through an innate lymphoid cell-IL-22 axis. Science 351 (6279), pp.1333-1338. (10.1126/science.aad9903)
- Morgan, M. et al. 2016. Sepsis patients with first and second-hit infections show different outcomes depending on the causative organism. Frontiers in Microbiology 7 207. (10.3389/fmicb.2016.00207)
- King, A. , Hopkinson, J. B. and Milton, R. 2016. Reflections of a team approach to involving people with dementia in research. International Journal of Palliative Nursing 22 (1), pp.372-377. (10.12968/ijpn.2016.22.1.22)
- Dickinson, P. et al., 2014. Whole blood gene expression profiling of neonates with confirmed bacterial sepsis. Genomics Data 3 , pp.41-48. (10.1016/j.gdata.2014.11.003)
- Eberl, M. et al. 2014. Pathogen-specific immune fingerprints during acute infection: The diagnostic potential of human γδ T-cells. Frontiers in Immunology 5 572. (10.3389/fimmu.2014.00572)
- Davey, M. S. et al., 2014. Microbe-specific unconventional T cells induce human neutrophil differentiation into antigen cross-presenting cells. Journal of Immunology 193 (7), pp.3704-3716. (10.4049/jimmunol.1401018)
- Smith, C. L. et al., 2014. Identification of a human neonatal immune-metabolic network associated with bacterial infection. Nature Communications 5 4649. (10.1038/ncomms5649)
- Raby, A. et al. 2013. Targeting the TLR co-receptor CD14 with TLR2-derived peptides modulates immune responses to pathogens. Science Translational Medicine 5 (185) 185ra64. (10.1126/scitranslmed.3005544)
- Cohen-Bendahan, C. C. C. et al., 2005. Is there an effect of prenatal testosterone on aggression and other behavioral traits? A study comparing same-sex and opposite-sex twin girls. Hormones and Behavior 47 (2), pp.230-237. (10.1016/j.yhbeh.2004.10.006)
Events
Podcasts
Dr James McLaren took part in an episode of the Discovery Matters podcast to discuss the role of single cell sequencing in detecting sepsis:
Discover Matters - Detecting sepsis: the role of single-cell
Professor Peter Ghazal took part in an episode of the Lancet infectious disease series:
Combating Childhood Infections in LMICs: evaluating the contribution of Big Data
World Sepsis Day 2020 - webinar
Recording of our World Sepsis Day 2020 webinar.
Talking about Sepsis
This preview event took place on Wednesday 20 June 2018 in the 'Goldilocks Ward' of the new Sepsis Engagement Centre.
The event was very well attended with over 60 people from Cardiff University, Wales Gene Park, Cardiff & Vale UHB, Sêr Cymru, Welsh Government and The UK Sepsis Trust in attendance.
See more information about the Talking about Sepsis event.
View event Talking about Sepsis programme.
World Sepsis Day 2019
Sepsis: a spotlight on what can happen to mum and baby
Sepsis is a life threatening condition from infection, that can affect anybody at any age.
However, it is more common in vulnerable populations such as the very young and the very old. What is often not recognised is the significance of sepsis in pregnancy.
At the event we told Amanda’s story about a mother and baby who were severely affected by sepsis.
This was a free event open to all and took place on Friday 13 September 2019 in the seminar room and Sepsis Engagement Centre at the Sir Geraint Evans Cardiovascular Research Building at the University Hospital of Wales.
Event feedback:
'Excellent microbiology talk - very good illustrative case with patient perspective'
'Excellent varied programme, particularly enjoyed the patient’s story'
'Wonderful clinical simulation'
'A privilege to join the discussion and an invaluable insight into the global challenges of tackling sepsis'
Public engagement
Sepsis Engagement Centre
We seek to promote interaction between patients, researchers, and clinical staff through the Sepsis Engagement Centre, physically located in the Sir Geraint Evans Cardiovascular Research Building, acting as an interaction and training hub. Planned audio-visual exhibitions include “The sepsis life cycle”, an exhibition of simulation wards with featured displays of neonatal intensive care unit (NICU), paediatric intensive care unit (PICU), adult intensive care unit (ICU), and an exhibit for scientific understanding of current and planned future medical tests and treatments for sepsis.
The Sepsis Engagement Centre aims to engage through outreach events and to promote patient and public involvement (PPI) for making a real difference in our research and the clinic for saving lives against sepsis.
Read more about the preview event that was held for the Sepsis Engagement Centre on 20 June 2018.
Why the 'Golidlocks Ward' - The Goldilocks fairy tale
The Goldilocks fairy tale was first recorded in narrative form in 1837, in a collection of essays by Robert Southey titled “The Doctor.”
As in the house belonging to the three bears, the Goldilocks Ward has three beds, from our tiny neonatal cot to an adult hospital bed. The distinct zones provide crucial opportunities for simulated training and research. They represent:
- Neonatal Intensive Care Unit (NICU)
- Paediatric Intensive Care Unit (PICU)
- Adult Intensive Care Unit (ICU)
The ‘Goldilocks principle’ means to strive for what is ‘just right’. Our interactive display explores the application of this principle to precision medicine and the antibiotic treatment of sepsis - getting just the right medicine to the right patient.
Sepsis is caused by an unbalanced immune reaction in our blood to fight infection. The main pathogens that can trigger sepsis range in size Fungal/Yeast, Bacterial, Viral.
A community action for getting involved to be involved in sepsis awareness and research
Central to helping us reach our goals are Lay Advisory groups for neonatal, paediatric, and adult sepsis, respectively. The role of our Lay Advisory groups is to help review research priorities, identify new lines of research, give input into research proposals (lay summaries in particular) and impact statements and website content, as well as contributes to the dissemination of research findings to relevant target groups.
Lay advisory involvement for project sepsis is underway with opportunities to join the pool of lay advisors in our community action against sepsis. We especially welcome those affected by sepsis either directly, as former patients, or indirectly as family members of former patients as well as those who wish to get involved out of general interest.
If you would like to find out more about patient and public engagement, please contact: projectsepsis@cardiff.ac.uk
Our lay advisory community
- Terence Canning (aSEP)
- Nicola Madoc-Jones (nSEP)
- David Madoc-Jones (nSEP)
- Holly Powell (nSEP)
- Tracey Laight (aSEP)
- Jacqueline Mason (aSEP)
- Alan Brown (aSEP)

Our funding
This project is part-funded by the European Regional Development Fund through the Welsh Government.
Schools
Images
Next steps
Research that matters
Our research makes a difference to people’s lives as we work across disciplines to tackle major challenges facing society, the economy and our environment.
Postgraduate research
Our research degrees give the opportunity to investigate a specific topic in depth among field-leading researchers.
Our research impact
Our research case studies highlight some of the areas where we deliver positive research impact.