Potential new treatment for advanced cancers
25 January 2018
A potential treatment for therapy-resistant breast cancer patients has been uncovered by researchers at Cardiff University.
The European Cancer Stem Cell Research Institute, based with Cardiff University, has repurposed a current cancer therapy, TRAIL, to find a new treatment for advanced cancers that are resistant to anti-hormone therapy.
Up to 75% of women diagnosed with breast cancer will have a cancer driven by oestrogen signalling and almost all of these women will receive anti-hormone therapy, like Tamoxifen or Aromatase inhibitors, to treat their cancer. Unfortunately, up to 40% of patients receiving these hormone therapies will develop a resistance to them, leading to relapse with aggressive cancer.
Dr Luke Piggott, European Cancer Stem Cell Research Institute at Cardiff University, said: “Part of our research focus is to develop new therapies, with low levels of side effects, for breast cancers that are resistant to anti-hormone treatments.
“TRAIL has already been tested in multiple types of cancer, but hasn’t yet proved beneficial to patients. But we believe we have demonstrated that patients who develop resistance to treatment will benefit from TRAIL therapy, as we have identified specific changes in the cancer cells from these patients, which mean that their tumours become sensitive to TRAIL treatment.
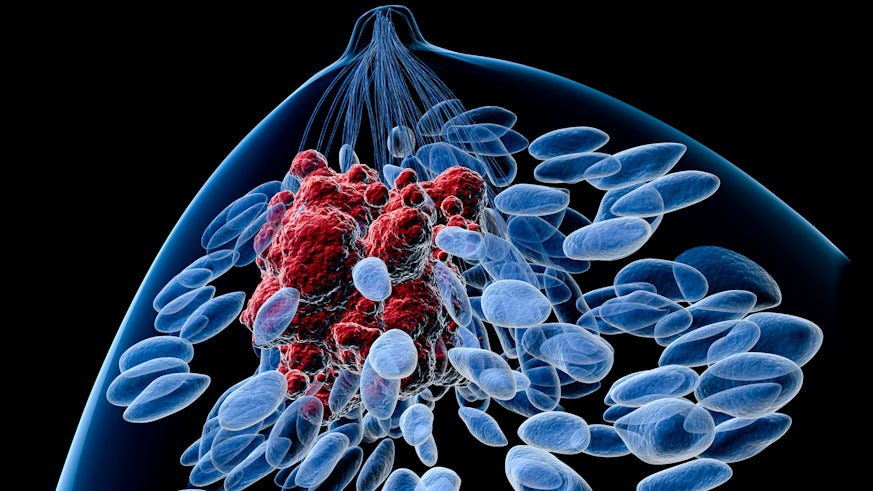
“Additionally, we have shown in this patient group that TRAIL treatment targets a specific type of cell in a tumour called a cancer stem cell. Cancer stem cells differ to the other cancer cells, as they are the cells responsible for initiating tumour growth and spread, and have also been shown to be resistant to therapy.”
Dr Richard Clarkson’s team of researchers at the European Cancer Stem Cell Research Institute tested TRAIL on tumour samples collected from cancer patients who had developed resistance to anti-hormone therapy.
Their findings showed that TRAIL selectively killed cancer stem cells from these patients but that tumours that had not developed resistance to tamoxifen were unaffected by TRAIL.
Dr Richard Clarkson said: “Cancer stem cells are the cells responsible for relapse and for the spread of cancer, so by targeting these cells, along with the bulk of the tumour, we could transform the way we treat cancer, especially for those that are resistant to anti-hormone treatments.”
82 percent of the anti-hormone resistant tumour samples showed a significant response to TRAIL, whereas only 8 percent of tumour samples that had not previously seen anti-hormone therapy responded.
The experimental models showed tumour shrinkage after being treated with TRAIL and there was also a reduction in the number and size of tumours that have spread to other organs, a process known as metastasis.
Dr Clarkson added: “Although we have more research to do before this new drug gets into clinic, TRAIL represents a very promising therapy for a population of patients where there is currently very few options.”
