Schizophrenia: from new brain cells to the immune system
8 Mehefin 2017
We still don’t really know much about one of the most common psychiatric diseases – schizophrenia. However, my research, and that of many others, shows things such as neurogenesis (formation of new neurons) and the immune system are all involved in this challenging condition.
Genetic risk of schizophrenia
Schizophrenia is a complex disease, with symptoms including hallucinations and delusions, emotional and motivational changes, and social interaction problems. Even though up to 1% of the UK population suffers from it, little is known about what causes schizophrenia.
We do know, however, that there is a large degree of heritability, although environment certainly plays a role, too. In identical twins, if one sibling has schizophrenia, there is at least a 50% chance that the other sibling will develop the disease as well.
Colleagues at the MRC Centre for Neuropsychiatric Genetics and Genomics, are experts of trying to work out the genetic risk factors for schizophrenia. Through looking at the genomes of large numbers of schizophrenia patients, they have identified over 100 genes that when lost, or duplicated, increase the risk of developing the disease. Some of these are well known genes in brain development and functioning. Others, we know little about.
At Cardiff University’s Neurosciences and Mental Health Research Institute (NMHRI), we use rodents that possess some of these genetic risk factors to look at the behavioural, structural, and cellular changes in such genes. My particular research focus is examining the effects of schizophrenia risk genes on adult neurogenesis.
New cells for old brains
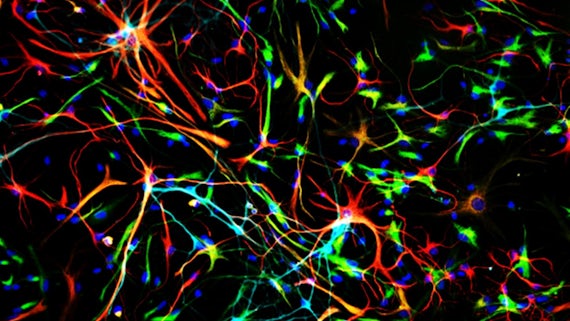
For a long time, the dogma in neuroscience has been that you can’t create any new brain cells as an adult. However, we know now that every one of us is generating new neurons every day through a process called adult neurogenesis.

These cells are only made in certain brain areas which contain the stem cells that can produces new neurons. The main place this happens is in the hippocampus, a brain structure important for learning and memory, information processing, and involved in emotional regulation.
New neurons are specifically involved in a number of processes. One of their most important roles is pattern separation. That is, the ability of the hippocampus to distinguish between two similar, but different, stimuli. These cells are also important for the person’s ability to forget things and, in some forms, regulating emotion.
Effects of schizophrenia on adult neurogenesis
Why is this important in schizophrenia? We know from post-mortem studies that neurogenesis is altered in schizophrenia patients. We also know that some of the anti-psychotic drugs patients take can change neurogenesis. More importantly, many of the processes with which the newly born neurons are involved are closely related to the symptoms of schizophrenia. For instance, if pattern separation goes wrong, this could lead to confusion and delusions, as everyday stimuli are misinterpreted by the brain. Similarly, problems with forgetting and emotional regulation could lead to many of the behavioural changes seen in this psychiatric disorder.
Colleagues and I have looked at the effects of three different schizophrenia risk genes, all with very different functions. What we found was a mixed picture; deletion of one risk gene increased neurogenesis and loss of a second decreased it, whereas the third gene studied didn’t have any effect. What this tells us most of all is that, unsurprisingly, things aren’t as simple as we might have thought. The specific gene I am working on showed an increase in neurogenesis. Further research led to an unexpected destination: the immune system, and the way it may regulate adult neurogenesis.
The immune system in schizophrenia
The immune system in the brain consists of cells called microglia. These cells are important for more than just fighting infection. In many ways, they are the gardeners of the brain. They trim connections that are no longer being used, tidy up dying cells, and guide and control the outgrowth of new neurons. (I wrote about neuro-immunology in a previous blog.)
In the past few years, there has been a growing realisation that there are alterations in the immune system in schizophrenia. Scanning patients to look at their microglia has produced mixed results, in some patient groups they are more activated, in some groups less so. As more and more data appears, it is becoming clear that there’s something going on with the microglia.

My research showed that animals carrying this particular schizophrenia risk gene did not produce any more cells, but still ended up with more neurons. This is not as strange as it seems, as the brain makes more neurons than it needs and then trims it down to the required number by keeping only the ones that work well. It would seem that this trimming down process is disrupted in the presence of this risk gene.
This is where the microglia come in. By isolating stem cells from the hippocampus and growing them in a dish, I could both observe and manipulate the formation of the new neurons. When I grew cells from non-at risk animals, but removed the microglia, they behaved exactly like the cells isolated from schizophrenic risk animals, having more surviving neurons. What this suggests to us is that there is something wrong with the microglia in our animals, and this is causing the differences in neurogenesis as the microglia are unable to trim the excess neurons.
So, where next?
Identifying what is going wrong with the microglia and what effects it has on other processes in the brain (such as the structure of neurons) is our next area of research.
More generally, our work is telling us more and more about schizophrenia. What it mostly boils down to is: it’s complicated. There is no single gene that causes schizophrenia – no single mechanism causes the symptoms. However, looking at specific aspects such as neurogenesis and microglia functioning, and the effects of genetic risk factors, can tell us more about the mechanisms of the disease and hopefully help with better treatments.
Visit The Brain Domain to read Niels' next blog entitled: 'What is neuroimmunology and why should I care?'

