Magda's cancer research story
"I was already working in cancer when my sister died of sarcoma in 2013 at the age of 41."
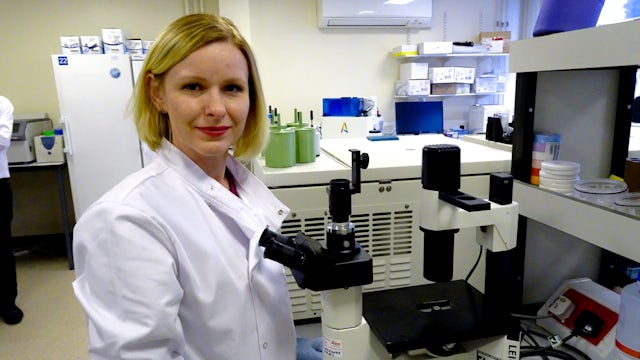
Magda Meissner is a researcher and clinician, but her cancer story, as for so many people, is much more personal.
"My sister Ivona didn’t tell us for a long time that she had a lump in her leg. She only went to the doctor when she had pain - the ultrasound showed up something suspicious."
As an oncological registrar (a doctor who had already specialised in treating cancer), Magda was aware of sarcoma, and knew how serious a diagnosis could be.
"Once I knew it was sarcoma, I called all my friends from medical school to find out where the best place was to treat it in Poland (where Ivona was living). In Warsaw, they did a scan of her chest and found metastatic tumours on the chest. She was diagnosed with advanced stage cancer.
"She had to have several rounds of chemotherapy. At first, it worked. The tumours disappeared and then she had an operation to remove any remaining cancer. She was clear and happy but then a scan showed new tumours.
"The next round of chemotherapy just wasn’t really controlling the cancer. It was growing and growing. I was on maternity leave and so I was there as much as possible. I was helping as much as I could, but the chemo stopped making a difference.
"Normally if you diagnose at that stage, survival is between 12 months to 18 months and Ivona had maybe 18 months.
"Chemotherapy was effective at first but the effect didn’t last long. It felt like it gave us false hope."
Magda has first-hand experience of what the lack of a spotlight on a disease does. Sarcoma is a rare form of cancer affecting tissues such as muscles, bones and joints. Its rarity alone would be challenging enough, but it also has between fifty and eighty subtypes, further complicating the picture.
"Its rarity means that people with lumps might ignore them, as most lumps are benign. The diagnosis of sarcoma can be challenging, and sometimes GPs and surgeons don’t know what to do with it. The wrong management of sarcoma can then lead to its spread."
As well as treating rare cancers like sarcoma, studying and understanding them is challenging too. Funding for research is competitive, and with the added complication that clinical trials may be harder to coordinate, the situation is often frustrating.
"It’s very difficult to do trials in rare cancers – pharma companies may not want to invest because it’s not seen as profitable, and so it’s important to work with charities and donors, and to make people aware, to get doctors on board (which is hard when they sometimes see only 1 sarcoma patient in many years of practice).
"Research on sarcoma needs more trial centres – across the whole of the UK and internationally. I feel that every patient has the right to access trials wherever they live and at the moment it depends on whether the centre near them is part of the specific trial – then the patient might not have that opportunity. Not everyone can go to London, and people don’t want to be travelling for three to five hours every week.
"Ivona’s experience is a constant reminder to me of the patient perspective and of the urgency of the situation. I want to accelerate these trials and get progress fast."

It’s clear that Magda is focused on directly helping patients, but she also has a broad vision of how to achieve that.
"Being a clinician, close to becoming an oncology consultant, I want to make the patient experience of cancer so much better - from screening to diagnosis to treatment.
"My aim is to continue as a clinical academic, working in clinics and in research, setting up trials, collecting samples, developing biobanks and learning more about the biology of cancer from trials."
Magda's PhD looked at resistance to treatment in breast cancer. She's now waiting to start a clinical trial, to test immunotherapy as a treatment for sarcoma patients.
"There hasn’t been much investment in treatment for sarcoma. Chemotherapy is currently the main treatment for sarcoma. It affects all the dividing cells in your body - your normal cells and the cancer cells - which can cause side effects.
"Immunotherapy stimulates your own immune system to fight cancer. This trial would be a big step for sarcoma research. There is no immunotherapy for sarcoma patients in the UK, and there is a low response rate to chemotherapy.
"Immunotherapy has been explored for so many different types of cancer so why not for sarcoma?"
Just as Magda is applying her knowledge about one cancer to another, the cancer research community at Cardiff University is highly collaborative, working together across types of cancer and across types of science – from the microscope to the bedside.
1 in 2 people in the UK will get cancer in their lifetime but there are more than 200 types of cancer. It is vital that we have a culture that develops expertise across the board, sharing ideas and facilities for the biggest impact.
To flourish in this community and the wider competitive environment of research, “non-bench” skills, like communication skills and grant writing, are essential.
The Future Leaders in Cancer Research (FLiCR) programme provides these skills for early career researchers. What good is ground-breaking research if it’s not shared, and what use are science-shifting findings if they are not developed?
This carefully targeted career development enables talented scientists across cancer research to enhance, share and build on their ideas. Your support is therefore enabling them to make the move from theoretical science to drug development, policy changes, and even new clinical trials. You might not be providing test tubes and petri dishes, but FLiCR donations give our researchers the opportunity to make their research more global, more transferrable, more impactful.
Magda is a graduate of the Future Leaders in Cancer Research programme. And now, because of your support, she successfully applied for a fellowship to do a clinical trial in immunotherapy as a treatment for sarcoma.
"We are going to do two things. We are going to give sarcoma patients an immunotherapy drug to see if we can help the body to fight cancer. And we are also going to give patients something which stops a protein in the body from masking the cancer – so it should make the cancer visible and recognisable to the boosted immune system.
"Because sarcoma is a rare cancer this research will need to include centres and networks across the UK and internationally. And because it’s rare, any application for funding needs to be very compelling.
"Because of FLiCR, I got guidance from senior academics and I got to know other researchers across Cardiff University like Martin Scurr, a fellow FLiCR participant, who works in immunotherapy and who I will be working with. Furthermore, I developed an international network of those who work in rare cancer and clinical trials through a competitive course on clinical trial design that FLiCR donations enabled me to take part in. Even the fellowship application itself was strong because of FLiCR training."
Crucially, because Magda will be running a clinical trial, sarcoma patients will be impacted by her research immediately. That’s the power of your support. It allows talented and determined people to move towards their goals quickly, which means hope for patients and families now and in the future.

''I'm working for a day when a cancer patient can have a blood test to find out what mutations they have and what treatment their body will respond to. These hopes aren't far off. This future is within our grasp. And I want to work hard to get there fast.''

How you can help
Thank you for choosing to support Cardiff University. Every contribution – no matter the size – makes a lasting impact on our world-leading teaching, learning and research.



