Preventing fibrosis
9 February 2018
Researchers at Cardiff University and the Wales Kidney Research Unit have discovered a potential new method for preventing the process that causes scar formation in organs.
The new research, in collaboration with the University of Exeter and the Cleveland Clinic Lerner Research Institute, involves altering the cells responsible for wound healing and tissue repair and could lead to treatments that would prevent and even reverse organ fibrosis – a major cause of illness and death around the world.
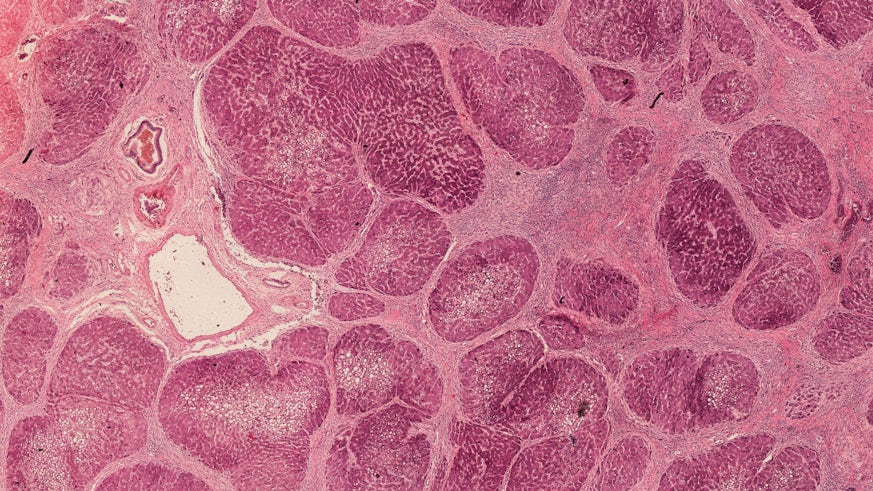
Fibrosis is the formation of excess fibrous connective tissue in an organ as part of a reparative or reactive process. This biological process can lead to permanent organ damage and chronic disease. Fibrotic diseases include cardiac and pulmonary fibrosis, atherosclerosis, asthma, cirrhosis and scleroderma.
During their laboratory tests, the team discovered that a protein previously thought to simply break down sugar chains can be used to make alterations to the RNA of cells responsible for wound healing and tissue repair, radically affecting their function.
Dr Soma Meran, from Cardiff University’s School of Medicine and the Wales Kidney Research Unit, said: “We were amazed to discover that the protein Hyaluronidase-2 can bind to RNA in a cell and alter its activity. In the case of the cells responsible for fibrosis and scar formation, we can potentially use this technique to stop them from producing scar tissue. This opens up exciting new research avenues in the study of fibrosis.”
The team’s particular interests at the Wales Kidney Research Unit relate to the prevention and/or reversal of chronic kidney disease, which cannot currently be reversed and consumes approximately 3% of the NHS budget. Many of these patients ultimately require dialysis or kidney transplantation, and these treatments are associated with significant risks and complications.
The next phase of the research will be to further investigate the structure of Hyaluronidase-2 to identify what makes it travel to a cell nucleus and influence genetic material. In the future the team hopes to develop synthetic proteins that mimic the beneficial effects of Hyaluronidase-2 for development in therapeutics.
The research was funded and supported by the Medical Research Council.
The paper ‘Nuclear hyaluronidase 2 drives alternative splicing of CD44 pre-mRNA to determine profibrotic or antifibrotic cell phenotype’ is published in the journal Science Signalling.
